For many hospitals, exceeding resources due to high volumes of COVID-19 is not a matter of if, but when.
A model from the University of Pennsylvania is helping hospitals predict how close that when might be.
[See the app here.]
From STAT:
CHIME (“Covid-19 Hospital Impact Model for Epidemics”), built by Penn’s Chivers and others in “predictive healthcare,” is a basic epidemiological tool of infectious disease spread called a SIR model. It takes what’s known about the number of susceptible (S) people in an area (which for Covid-19 is everyone, since no one has immunity to the new coronavirus that causes it), the number of infected (I) people, and the number of recovered (R) people (who are presumed to be immune from subsequent infection). Because of the disastrous rollout of Covid-19 testing in the U.S., the researchers assume that only 15% of cases have been detected (but say it could be even lower).
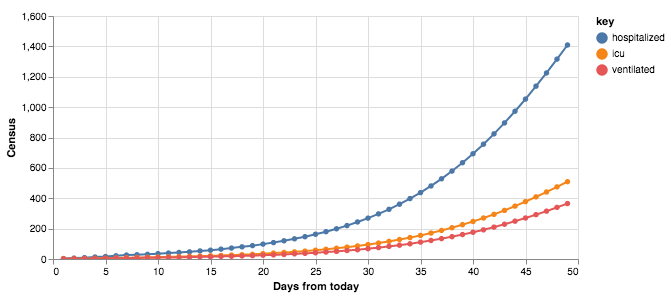
The model then uses the best current estimates of how long someone is infectious (14 days); how many new cases each infected person causes (called the effective reproduction number, it’s about 2.5); the percentage of Covid-19 patients who need to be hospitalized (5%, reflecting the fact that most people have only mild or moderate illness); the percentage who need to be in an ICU (2%) or on a ventilator (1%); and the length of stay for each of these three.
The team built the model to help administrators at Penn’s hospitals determine how many beds and other resources they are likely to need in the coming weeks. Using current data (31 known cases in the region, two patients hospitalized), for instance, CHIME projects that by late April, 40 days from now, there will be 100 Covid-19 patients in the hospital every day, 50 in the ICU, and 30 on ventilators. By early May, 50 days hence, the figures are 300, 150, and 75, reflecting the exponential growth in the epidemic. The model also projects the daily number of new cases in each of these categories: 60, 25, and 12, respectively, 50 days from now.